Systemizing Healthcare: The Integrator Role
This is Part 2 of a Four-part Leadership Transformation Series (LTS). Read Part 1 Here.
Transformation in healthcare is personal: it requires the transformation of health system leaders. This LTS begins to speak to key differences in some of the fundamentals of transformational vs traditional leadership in healthcare.
This article focuses on the changing role delineation of leaders.
The leadership need for ‘the Integrator’ is re-shaping traditional CEO and COO roles.
A few decades ago, the role of ‘the Integrator’ in healthcare leadership did not exist – at least not in the form needed today. Unlike roles with new names – CTO, CMIO, CPHMO, etc. - the same titles of CEO or COO may be used for a healthcare system, yet the shapes of these roles bear little resemblance to those with the same titles used in a hospital or other ‘vertical.’
While a hospital administrator/CEO is expected to stay close to the pulse of acute care operations, the system CEO is expected to transcend operations to assure an aerial view/perspective, i.e., to become more visionary and system-focused. The transition from hospital to system requires a view that is less entrenched with how we have run hospitals and more focused on the population served. Despite use of the same title for both roles, it is the difference between being ‘tied down’ and ‘freed up.’
‘Pushing up’ the system CEO role creates space between the maximization of operations in an individual vertical, e.g., hospital, physician practices, and pre- and post-acute services (possibly insurance) and optimizing a system of care for a population. The integration leadership challenge for health systems involves numerous business verticals or silos. But this is only a start: to ‘systemize’ healthcare systems, integration of IT/digital, consumer engagement and culture to a new level are needed. In this space, created between the elevated CEO visionary role and numerous operating entities, is the work to ‘systemize.’
Enter the Integrator.
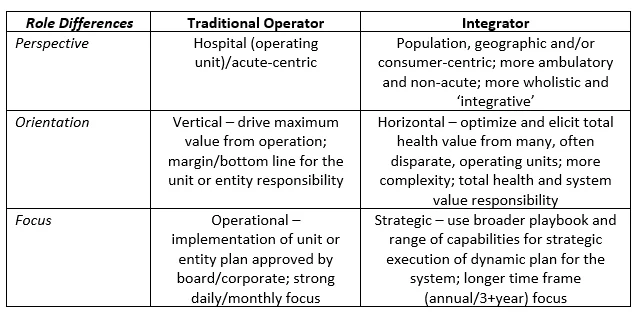
The Integrator is responsible for making sure that ‘strategy execution’ is not an oxymoron. While responsibilities of the Integrator role are clearly shared among the leadership team, some key differences in the healthcare system Integrator role, often personified in the COO role for a larger system (or a conflicted CEO in a smaller system) are noted below.
The Integrator role cannot succeed without support at the highest level. Perhaps more than in other industries, healthcare often struggles with this deliberate separation of duties between system CEO and COO. The problem is particularly acute in smaller communities where some want ‘a hospital or two to become a system,’ while others hold fast to remaining ‘the hospital we have always been.’ What is best for a hospital and some of its immediate stakeholders, e.g., providers who are hospital-based (and hospital board members who are vulnerable to influence by them), is not always what is best for a system tasked with serving a population.
For example, it is not enough to decide “we are no longer a hospital, we are a system;” all the stakeholders need to truly commit. Without serious fortitude to weather the inevitable emotions of resistance and perceived loss during the key transitions in this transformation, a board is susceptible to panic somewhere between an “ending” and “the neutral zone,” as Bridges (in his book Managing Transitions) refers to the first two phases of a transition. In the third phase, the distinction between a start and a beginning is the difference between announcing a formal decision by a few and embracing an emotional commitment by many. The development of new values, attitudes and identities for a beginning takes time. Because the Integrator role straddles both start and beginning, the Integrator often gets caught in the middle.
So What?
Two implications stand out for leaders and their key stakeholders to whom they are accountable. One is the increased inward need to reconcile inevitable conflicts at the horizontal-vertical intersections to clarify goals, priorities and role delineation among healthcare leaders. This ‘managing the matrix’ competency is not well understood nor explicitly taught.
A second is the significant outward need for ongoing dialogue among stakeholders about expectations for the Integrator role. If the system CEO is expected to spend time with people associated with the activities noted in the ‘Integrator’ column above AND ALSO be as available and visible to hospital stakeholders as the traditional hospital-operator-who-had-the-same-title, then s/he is set up to fail.
In short, the job of ‘systemizing healthcare’ requires new and more diverse competencies of the Integrator role - but this is not sufficient. True systemization also requires much time, communication and effort to assure other stakeholders understand and embrace the different expectations of this role – to embrace a new beginning, not just a start, of the journey.